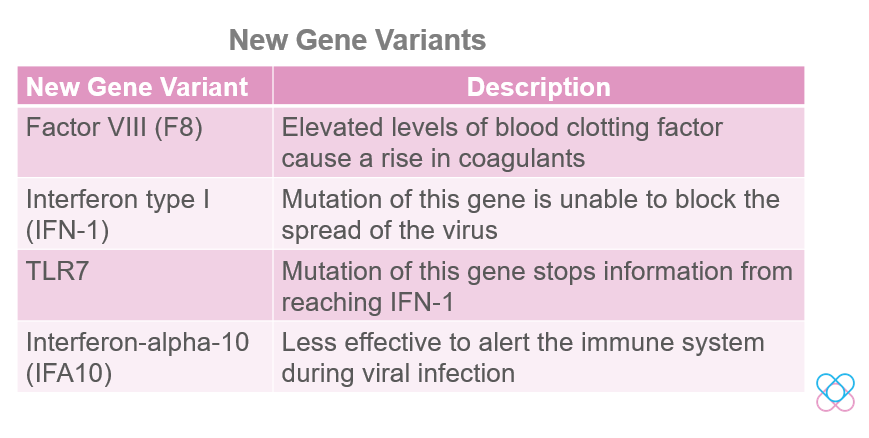
Previously, we have discussed gene variants in interleukins, HLA and CD14. We now know how these variants may affect the severity of COVID-19 infection among different individuals. In this current article, we will look at other gene variants that may increase the risk of COVID-19 severity.
READ ALSO: How Genes Make Us More Susceptible To Coronaviruses
—
Inheritance strongly influences both the susceptibility to infections and immune-mediated diseases. In recent news, scientists have discovered new genetic variants in patients who suffered from severe COVID-19. These patients may have genes that predispose them to one of these problems; either the failure to block the virus from making more copies of itself, excessive inflammation, or blood clotting.
COVID and Blood clot
Blood clots in our bodies help us to stop bleeding during an injury. An injured blood vessel will produce proteins. Then, the proteins call upon platelets and other clotting factors to the site to fix and heal the wound.
However, some COVID-19 patients may develop abnormal blood clotting. This means that there is a blood clot even without an injury. If the blood clot blocks the blood vessel, the tissue around the blood vessel would lack oxygen. As a result, the cells in that area may die. Additionally, several health risks including stroke, heart attack, and kidney failure could also happen[8].
A study showed that changes in the key genes of blood clotting Factor VIII (F8) cause elevated levels of coagulants. As a result, patients may develop severe forms of COVID-19[5]. Regulation of F8 is dependent on the von Willebrand factor (vWF), a molecule that carries protein factor F8. The increase in vWF levels leads to an increase in F8, which causes blood clotting[4].
It is still unsure the exact reason for the blood clot; however, research has found that it could be due to one or a combination of these mechanisms below[8]:
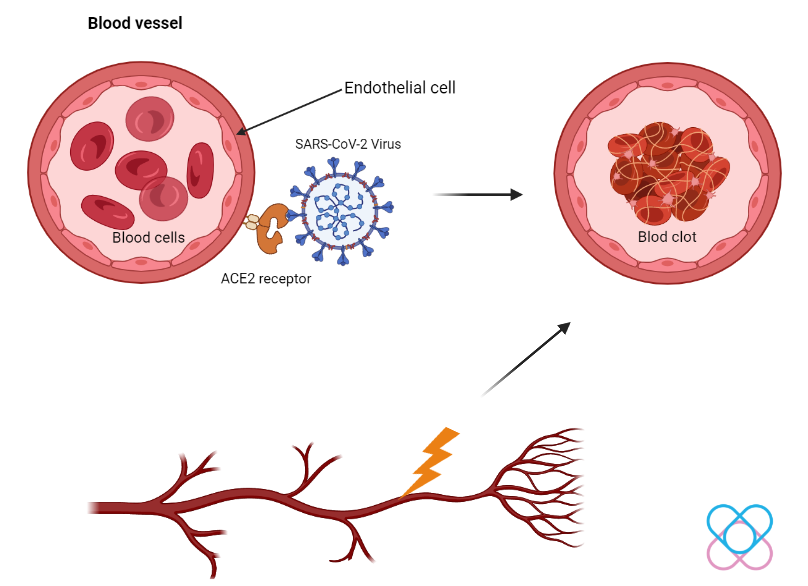
- Endothelial cells (cell lining in blood vessels) express ACE2, a protein that helps in SARS-CoV-2 viral entry. This allows the virus to attach and harm the endothelial cells, which trigger the blood clot.
- Damaging of the tissues around the endothelial cells due to the viral infection or immune response could also trigger clotting.
- Increased production of inflammatory molecules due to the viral infection could also activate clotting.
Interferon signaling pathway
Interferons serve to boost the immune response to viral infections. Interferon type I (IFN-1) provides natural immune defenses against viruses. Sensors in a cell such as TLR3, TLR7, and TLR8 activate the cytokines (IFN-I) when they detect viral RNA. Consequently, IFN-1 molecules will bind to their receptor (IFNAR1 & IFNAR2) and block the spread of the virus. Thus, this action stops the virus from making more copies of itself[7].
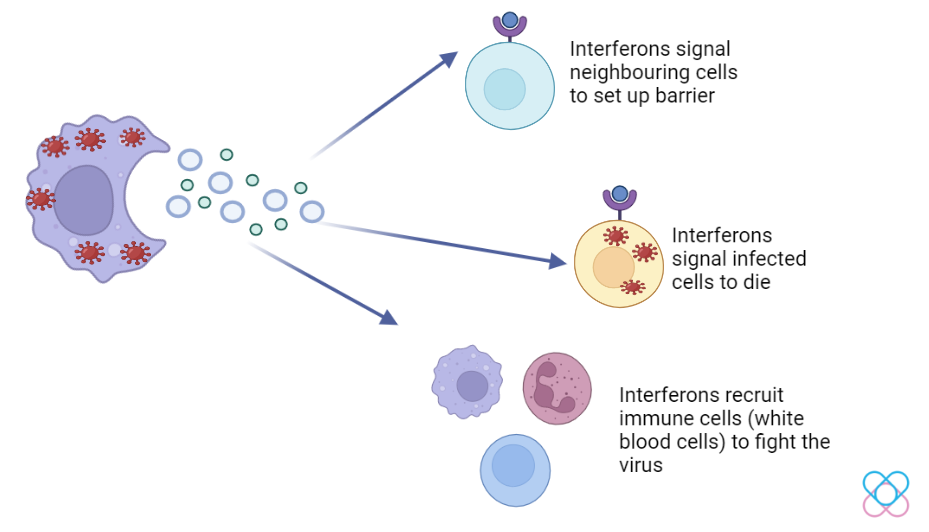
However, mutation of this gene is unable to block the spread of the virus which leads to severe COVID-19.
The sensor (TLR7) detects and informs IFN-1 to fend off the virus. In contrast, mutations in this gene stop the information from reaching IFN-1. This results in severe COVID-19.
Moreover, there is another gene variant called interferon alpha-10 (IFA10). This variant is less effective at alerting the body’s immune system during viral infection. A study reported that people with this variant are more likely to die from COVID-19[5, 7].
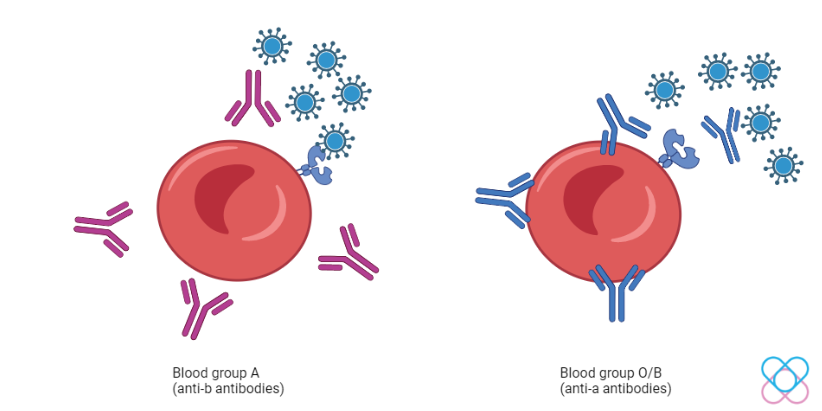
ABO Blood Group
Did you know that your blood group may also be a factor in the risk of COVID-19 severity? Different blood groups have different antigens on the surface of the cells produced by the gene FUT1. The antibodies will attach to their respective antigens. For example, blood type A has antigen A in which its antibody partner is an anti-B antibody[1].
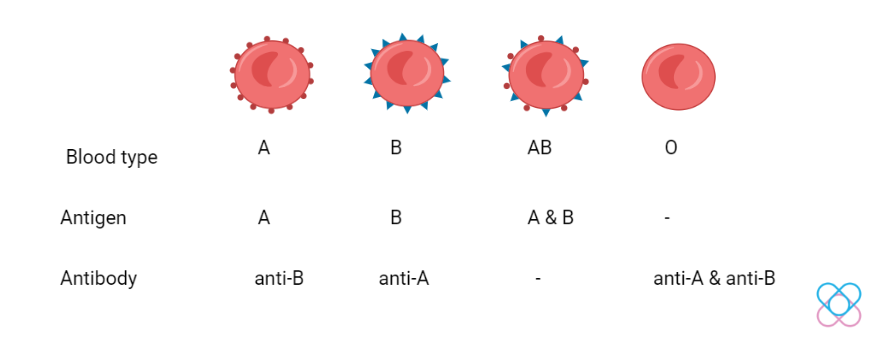
Individuals with blood type A have a higher infection risk while blood type O is lower. Blood type O and B individuals have anti-A antibodies. These antibodies block the S protein of the virus from attaching to the ACE2 receptor.
However, blood type O individuals are more protected against the virus than blood type B. This is because they both have different types of immunoglobulin (antibody). Blood type O is also associated with reduced abnormal blood clot incidents. Hence, blood group O individuals are granted more protection[3].
However, the molecular mechanism of the ABO blood group must be further studied so that we can better understand the association between the blood group and COVID-19 severity.
Conclusion
Ultimately, blood clotting factors and the immune system are among the many important parameters in our human body as they protect us from viruses such as SARS-CoV-2. These genetic variants allow scientists to look deeper at the genomic level of individuals. In the future, medicine can be tailored to target specific genes that cause the severity of the disease.
Discover your genetic predisposition in COVID-19 infection risk and severity with Project CoviDNA.
**The current Project CoviDNA does not include the genes above, it is still under consideration to be included in the future.
References
1. Anon. How is Blood Type (A, B or O) determined by genes? GB HealthWatch. Accessed 18th March 2022, from https://www.gbhealthwatch.com/Trait-Blood-Type-ABO.php.
2. Callaway, E. The Quest to Find Genes That Drive Severe COVID-19 (2021). Accessed 9th March 2022, from https://www.nature.com/articles/d41586-021-01827-w.
3. Gozman, L., Perry, K., Nikogosov, D., Klabukov, I., Shevlyakov, A. & Baranova, A. (2021). A Role of Variance in Interferon Genes to Disease Severity in COVID-19 Patients Front Genet. 12:709388.
4. Kamphuisen P.W, Eikenboom J.C, Bertina R.M. (2001). Elevated factor VIII levels and the risk of thrombosis. Arteriosclerosis, Thrombosis and Vascular Biology. May;21(5):731-8.
5. Kousathanas, A. et al. (2022). Whole genome sequencing reveals host factors underlying critical Covid-19. Nature.
6. Meffre, E. & Iwasaki, A. Interferon deficiency can lead to severe COVID (2020). Nature. Accessed 9th March 2022, from https://www.nature.com/articles/d41586-020-03070-1.
7. Mishra, M. Scientists Identify New Gene Differences in Severe COVID Patients (2022). Reuters. Accessed 9th March 2022, from https://www.reuters.com/business/healthcare-pharmaceuticals/scientists-identify-new-gene-differences-severe-covid-patients-2022-03-07/.
8. Seladi-Schulman, J. What to Know About COVID-19 and Blood Clots (2020). Healthline. Accessed 11th March 2022, from https://www.healthline.com/health/coronavirus-and-blood-clots.