On 11th March 2020, COVID-19 was announced as a global pandemic. It has struck and affected many people, especially the older people and those with chronic medical conditions such as diabetes, cancers and heart diseases[4]. In fact, it was reported that diabetes is ranked as the second most prevalent comorbidities (more than one disease/condition in a person) among COVID-19 patients, right after cardiometabolic diseases (e.g. cardiovascular disease, stroke)[10].
People with diabetes are facing double the challenges amidst the COVID-19 pandemic: higher risks of getting serious symptoms or mortality, and the need to pay extra attention in monitoring their blood glucose level daily.
In this article, we will be discussing how people with diabetes are heavily affected by COVID-19.
What is COVID-19?
Coronavirus disease (COVID-19) is a newly discovered infectious disease caused by the coronavirus (SARS-CoV-2), a respiratory pathogen. In January 2020, a novel coronavirus, known as SARS-CoV-2, was identified as the cause of a viral pneumonia outbreak in Wuhan (Hubei province), China[9]. On 11th March 2020, the World Health Organization (WHO) declared the mass infection caused by the “coronavirus disease 2019” (COVID-19) as a global pandemic[9].
Symptoms [2]
People with COVID-19 have a wide range of symptoms reported, ranging from mild to serious symptoms. Symptoms may appear 2-14 days after exposure to the virus. These symptoms show the person may have COVID-19:
- Cough
- Diarrhoea
- Difficult to breath
- Fatigue
- Fever or chills
- Muscle or body aches
- Loss of taste or smell
- Shortness of breath
Emergency warning signs of COVID-19:
- Trouble breathing
- Persistent pain or pressure in the chest
- Bluish lips or face
- Inability to wake or stay awake
Individuals with emergency warning signs should immediately sign for medical care.

Who is at risk?
People of all ages can be infected with the coronavirus. The International Diabetes Federation has reported that older people and people with pre-existing medical issues such as diabetes, heart disease and asthma, appear to be more vulnerable to become severely ill with the COVID-19 virus[6,11].
According to the latest research done by Longo et. al, (2020), it was reported that one-third of patients who have deceased due to COVID-19 were affected by diabetes mellitus in recent studies from China and the United States[9]. It was also stated that people with diabetes have a two-times increment in chances of dying as compared to those who do not have diabetes[9]. Also, a recent systematic analysis has also shown that people with diabetes and COVID-19 shows an increased risk of ICU admission and higher mortality rate[1].
Effects of COVID-19 On Diabetic Patients
When people with diabetes are affected by the coronavirus, it can be harder to treat due to the fluctuations in blood glucose and possibly the presence of diabetic complications[7]. This is because:
- The immune system tends to compromise, making it difficult to fight against the virus which means take a longer time to recover[7].
- The virus will try to elevate the blood glucose level in any environment[7].
How?
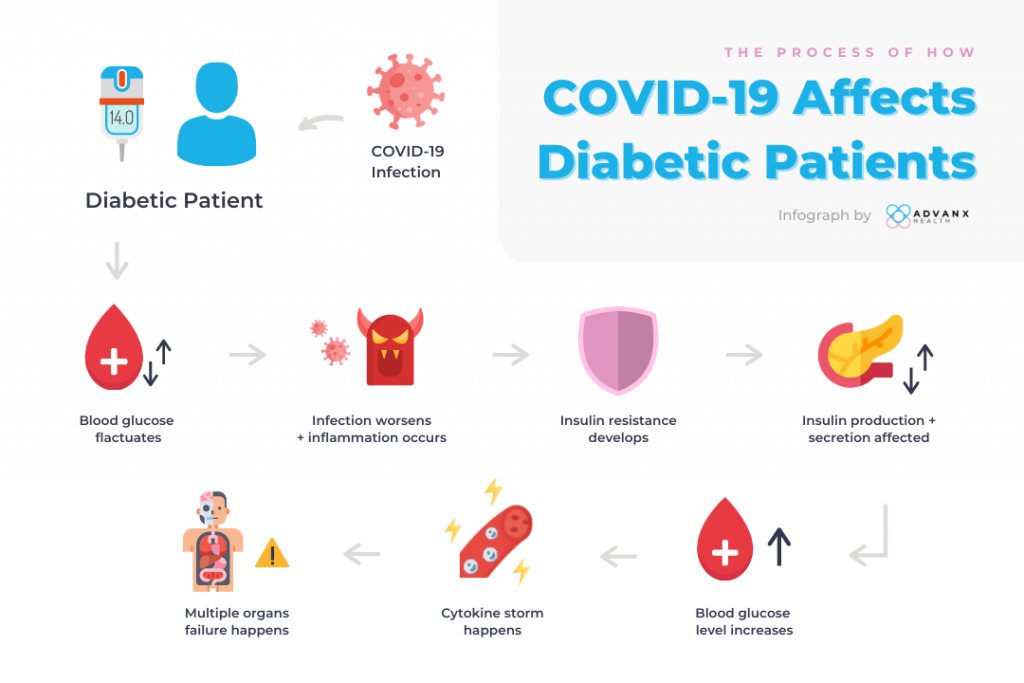
Once the people with diabetes are infected, it will likely aggravate the condition further. It will either:
- Increase the difficulty of blood glucose control
- Infection is more easily aggravated
As a result, this may lead to “cytokine storm” and acute inflammatory response[5].
Studies have shown that inflammation is closely related to the occurrence and development of diabetes. With the inflammatory cytokines, structural and abnormalities of the endothelial cells (a single cell layer that lines all blood vessels and regulates exchanges between the bloodstream and the surrounding tissues) are affected.
Hence, this can affect insulin transport in human tissues and cells, leading to insulin resistance[5].
At the same time, the inflammatory cytokines can destroy the pancreas beta-cells, which affect insulin secretion and production[5]. Eventually, this leads to the rise of blood glucose.
In the later stage of life for COVID-19 patients with diabetes, a “cytokine storm” will start rapidly, leading to the state of multiple organ failure, including liver and kidney failure[5].
What’s the cytokine storm? [9]
Cytokine storm is a severe immune reaction in which the body releases too many cytokines in the blood suddenly. It is also known as hypercytokinemia.
It is harmful to the body especially the body is presented with a large number of cytokines. It usually occurs during an infection, autoimmune condition, or other diseases or may occur after treatment when having immunotherapy.
Sometimes, the cytokine storm can be severe or life-threatening, as this can lead to multiple organ failure.
What should individuals with diabetes do?
Safety Measures[3]
For people with diabetes, it is important to take precautions and measures to avoid the virus if possible, such as:
- Practice social distancing
- Staying at home whenever is possible
- Washing hands regularly with soap and water (> 20 seconds)
- Use alcohol-based wipes/rubs
- Avoid non-essential travels

Wear mask and social distance 
Sanitize hands 
Wash hands regularly
Be Prepared[3]
Diabetic patients should also follow recommendations and communicate with their health practitioners. People with diabetes are advised to have adequate stock of medication and supplies of blood glucose apparatus in their home.
Besides, diabetic individuals will also need to always stay hydrated, monitor their blood glucose level and monitor the ketone bodies in the urine to prevent sickness.

Staying Active[3]
Regular physical activity should be encouraged for people with diabetes. Despite the restriction movement enforced by the government, physical activity workouts can be accessed via Youtube.
The intensity of the exercises should be tailored according to the capacity of the individuals.
Read More: How Type 2 Diabetes Affects Sports Recovery

Eat Healthily[3]
Diet is another thing that people with diabetes should be paying attention to. It is important to adhere to a regular well-balanced diet which consists of protein, fibre, vitamins and limited saturated fats. It is also recommended to go for low-glycemic index food (e.g. whole wheat pasta, brown rice) and limit the consumption of fried food.

What’s Next?
As the disease is new and there is a lack of data on how exactly people with diabetes are more susceptible to coronaviruses, it is difficult to confirm that people with diabetes who are infected with COVID-19 have a higher rate of mortality.
With more research and data available in the future, we hope to have a clearer understanding of this subject matter. By far now, the best way to avoid COVID-19 infection is to follow all the necessary safety precautions and measures given by the authorities.
Did you also know that your genetics may put you at high risk for developing diabetes? Find out more about your health risk in type 2 diabetes with DNA Explorer today!
References
1.Apicella, M., Campopiano, M., Mantuano, M., Mazoni, L., Coppelli, A., & Del Prato, S. (2020). COVID-19 in people with diabetes: understanding the reasons for worse outcomes. The Lancet Diabetes & Endocrinology, 8(9), 782-792. doi: 10.1016/s2213-8587(20)30238-2
2.CDC. (2020). Coronavirus Disease 2019 (COVID-19) – Symptoms. Retrieved 3 November 2020, from https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html
3.Cuschieri, S., & Grech, S. (2020). COVID-19 and diabetes: The why, the what and the how. Journal Of Diabetes And Its Complications, 34(9), 107637. doi: 10.1016/j.jdiacomp.2020.107637
4.Domenico, C., & Maurizio, V. (2020). WHO Declares COVID-19 a Pandemic. Acta Biomedica, 91(1), 157-160. doi: 10.23750/abm.v91i1.9397
5.Deng, M., Jiang, L., Ren, Y., & Liao, J. (2020). Can We Reduce Mortality of COVID-19 if We do Better in Glucose Control?. Medicine In Drug Discovery, 7, 100048. doi: 10.1016/j.medidd.2020.100048
6.Erener, S. (2020). Diabetes, infection risk and COVID-19. Molecular Metabolism, 39, 101044. doi: 10.1016/j.molmet.2020.101044
7.International Diabetes Federation. (2020). COVID-19 and diabetes. Retrieved 2 November 2020, from https://www.idf.org/aboutdiabetes/what-is-diabetes/covid-19-and-diabetes/1-covid-19-and-diabetes.html
8.Longo, M., Caruso, P., Maiorino, M., Bellastella, G., Giugliano, D., & Esposito, K. (2020). Treating type 2 diabetes in COVID-19 patients: the potential benefits of injective therapies. Cardiovascular Diabetology, 19(1). doi: 10.1186/s12933-020-01090-9
9. National Cancer Institute. (2020). NCI Dictionary of Cancer Terms. Retrieved 6 November 2020, from https://www.cancer.gov/publications/dictionaries/cancer-terms/def/cytokine-storm
10.Rogers, L., Lavery, L., Joseph, W., & Armstrong, D. (2020). All Feet On Deck—The Role of Podiatry During the COVID-19 Pandemic: Preventing hospitalizations in an overburdened healthcare system, reducing amputation and death in people with diabetes. Journal Of The American Podiatric Medical Association, 0000-0000. doi: 10.7547/20-051
11.Roncon, L., Zuin, M., Rigatelli, G., & Zuliani, G. (2020). Diabetic patients with COVID-19 infection are at higher risk of ICU admission and poor short-term outcome. Journal Of Clinical Virology, 127, 104354. doi: 10.1016/j.jcv.2020.104354